Congenital Heart Disease and GERD – How They Are Related.
by Saher V, Doctor of Medicine (M.D.)
What is Congenital Heart Disease?
Congenital heart disease is an abnormality in the structure of the heart that is present at birth and is the most common disorder affecting newborns. There are many types of congenital heart defects, ranging from simple to complex abnormalities. Infants can be born with a simple hole in the wall or septum that separates the heart chambers or they may have a defect in one of the heart valves that control blood flow into and out of the heart and through the heart chambers. Arteries may also be affected either because they are arranged differently or they have lost an important function such as failing to close down after birth, a condition referred to as patent ductus arteriosus. Other defects can be more complicated and combine abnormalities in several different heart structures such as the valves, vessels and heart muscle, as seen in a condition known as Tetralogy of Fallot. 1
Symptoms of Congenital Heart Disease
Congenital heart defects can cause a wide range of symptoms depending on the location and nature of the abnormality. Common symptoms are:
- Fast breathing or difficulty breathing because blood flow may not be carrying enough oxygen.
- Poor weight gain or failure to thrive because the baby may not be getting enough calories due to feeding difficulties.
- Sweating or damp hair or skin.
- Tiredness or fussiness.
- Frequent respiratory infections and breathing problems develop when the defect causes heart failure, a condition in which the heart muscle does not to pump blood as effectively as it should.
- Weight gain due to poor fluid circulation.
- Dry mouth or eyes are signs of dehydration and can also develop due to inadequate nutrition.
Gastroesophageal Reflux – GER and GERD
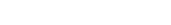
Infants with congenital heart defects may also develop problems with gastroesophageal reflux or GER in which acidic stomach contents can reflux back into the esophagus. This happens when the lower esophageal sphincter or LES, a circular band of muscle that separates the stomach from the esophagus, relaxes when it should stay closed. GER is the most common cause of vomiting during infancy. In healthy infants without any medical problems, these episodes of reflux may occur as much as 73 times per day and almost always completely resolve by 2 years of age. 2
In rare circumstances, GER may progress to troublesome gastroesophageal reflux disease or GERD, which occurs in only 5-8% of infants in general. 3,4
GERD, when severe, can lead to esophagitis or inflammation of the esophagus, and the infant may have behavioral changes such as irritability and disturbed sleep, arching, gagging, and may even refuse to eat. GERD also shares a number of symptoms experienced by infants with congenital heart disease such as weight loss and failure to thrive due to vomiting or poor intake of calories, as well as chronic respiratory or breathing symptoms such as cough, asthma or recurrent lung infections such as pneumonia.
Link Between GERD and Congenital Heart Disease
Congenital heart disease may predispose an infant to developing GERD because of the poor absorption of nutrients from the gastrointestinal tract that occurs with poor heart function, which often accompanies large defects. This deficiency in nutrient absorption can delay emptying of the stomach, which increases the likelihood of reflux. 5
Because of the overlap in some of the symptoms between congenital heart disease and GERD, and because GERD is not common in infancy, a diagnosis of GERD in an infant with a heart defect may often be overlooked.
Managing GERD
Lifestyle Changes
Certain lifestyle changes have been shown to improve symptoms of GERD. In a study of 50 infants with troublesome GERD, a two week trial of lifestyle changes found that by combining a milk-free diet, thickening feeds, anti-reflux positioning and avoiding tobacco smoke, symptoms significantly improved in 60% and resolved in nearly 25% of infants. 6
- Decreasing exposure to tobacco smoke. Though it is not known how much tobacco smoke contributes to GERD, nicotine is known to lower the lower esophageal sphincter pressure making it more likely to relax, causing reflux.
- Breastfeeding is encouraged because it may protect against regurgitation. 6 Smaller, frequent feedings, every 2 hours, 8-12 times a day may be the best approach for decreasing regurgitation. By expressing or pumping breast milk, the stress of a demanding feeding schedule can be shared between parents.
- Milk-free diet. Removing all cow’s milk from the baby’s diet and, if breastfeeding, removing cow’s milk protein and beef from the mother’s diet may improve GERD symptoms, which may be due to the infant’s intolerance of certain proteins. Formula fed infants should be given a “hypoallergenic” formula.
Thickening feeds – Adding oat infant cereal to either expressed breast milk or formula, up to one tablespoon per ounce of formula, appears to improve some of the symptoms of reflux. Rice cereal is no longer recommended because of possible contamination with arsenic. 7
However, in 2012, the Federal Food and Drug Administration or FDA issued a warning about thickening agents, because of reports that thickening formulas caused coughing and agents such as xanthan gum led to serious gastrointestinal problems in both premature and full-term infants. 8 Therefore, the decision to thicken your baby’s feeds should be discussed with your physician.
Positioning. Keeping an infant upright on a parent’s shoulder (not sitting or propped up in a seat) for up to 30 minutes after feeding seems to decrease the frequency of regurgitation.
All infants younger than 12 months should sleep on their backs (supine), even if they have reflux, because sleeping on their stomachs (prone) increases the risk of sudden infant death syndrome (SIDS). However, if reflux is severe, parents should discuss weighing the risks of reflux against the risk of SIDS with their physician.
- Acid suppressing medications are recommended only for severe cases of reflux, usually if there is evidence of esophagitis. Short-term trials of medications may be considered for infants with persistent symptoms such as poor weight gain, refusing to eat and irritability despite lifestyle changes.
- Surgery is rarely necessary and reserved only for severe cases of acid reflux.

Nutrition and Congenital Heart Disease
Special attention must be given to meeting the nutritional needs of infants with congenital heart disease. While specific approaches to feeding your baby may vary based on the type and severity of the heart defect, symptoms and whether the infant is recovering from surgery to correct the defect, the overarching goal is to supply enough calories to ensure a healthy physical growth pattern, because inadequate caloric intake is the main cause of growth failure.
The goal for determining how to best feed an infant with congenital heart disease is consistent weight gain. Most babies gain 1/2 to 1 ounce of weight per day. However, babies with heart disease tend to gain weight at a much slower rate. 9
The best situation is for your baby to take food by mouth. In some circumstances, breastfeeding may be the best option. In a small study involving seven infants with surgically repaired congenital heart defects who were of normal weight and otherwise healthy, breastfed babies were better able to coordinate breathing, sucking and swallowing and maintain good oxygen levels in their blood during feeding compared with those who were bottle fed. 10
However, another study found the infants who were bottle fed after heart surgery had the best growth curve and weight gain. Specifically, bottle-fed infants gained 20 grams per day vs. a 49 grams per day weight loss for infants who received only breast milk. 11
Parents should review the options of breast- vs. bottle-feeding with their physician and nutritionist and follow their infant’s weight gain to ensure that they are receiving the maximum benefit.
In some cases, oral feeding may be challenging for these infants who have symptoms from their heart disease. They may tire easily and their stomachs often hold smaller amounts of food or empty slower because of their heart condition. Respiratory infections can increase their breathing rate making it harder for them to coordinate their sucking, breathing and swallowing reflexes. 5 Fortunately, there are some strategies that can be used to optimize nutrition for these infants.
Recommendations on How To Optimize Nutrition for Infants with Congenital Heart Disease?

Parents should discuss with their physician and nutritionist:
- Increasing calories to higher concentrations, for example, 20 to 30 calories per day over a 3 -day span, has been shown to improve energy intake and weight gain following surgery. 12
- There are a number of methods that can be used to fortify breast milk or formula by increasing calories. Breast milk can be fortified with human milk fortifier (HMF) or commercial powdered formulas. Fortification can also be achieved by glucose polymers, microlipid or MCT oil and protein supplements. These options should be discussed with your physician or nutritionist. 5
- If GERD is suspected, the symptoms should be managed as previously mentioned. (see Managing GERD)
- Treating any heart symptoms with appropriate medications that reduce congestion and decrease the workload of the heart is obviously important.
- If weight gain is not occurring as planned, parents may need to combine oral feedings with feedings through a nasogastric tube (a tube that is inserted into the nose and passed into the stomach. In some situations, a tube may be inserted through a small skin incision directly into the stomach (gastrostomy) or into a section of the small intestine (jenunostomy). 5
At 6 months, discuss with your physician how to begin introducing solid into your baby’s diet. Special attention may need to be given to choosing high caloric foods that will help to maintain appropriate weight gain and growth.
 Canada
Canada South Africa
South Africa UK
UK EU & Int
EU & Int Ireland
Ireland Australia
Australia Brazil
Brazil New Zealand
New Zealand